what is the name of the measuring device used to assess intraventricular pressure?
Aortic stenosis is one of the nigh common valvular problems in the developed globe.1 Along with an crumbling population, the prevalence of aortic stenosis is expected to increase in the future. Although patients tin can be asymptomatic in early stages of the disease, symptoms that may be nowadays, especially in patients with a severe aortic stenosis, include shortness of breath; breast pain (angina), force per unit area, or tightness; and fainting.
Once symptoms are present, the prognosis is poor unless aortic valve replacement is performed promptly.two Before undergoing treatment, these patients can be examined with the Langston Dual Lumen Catheter from Teleflex, which measures simultaneous pressures across the aortic valve to help clinicians determine the pressure gradient and constructive orifice area (EOA) (Figure 1).
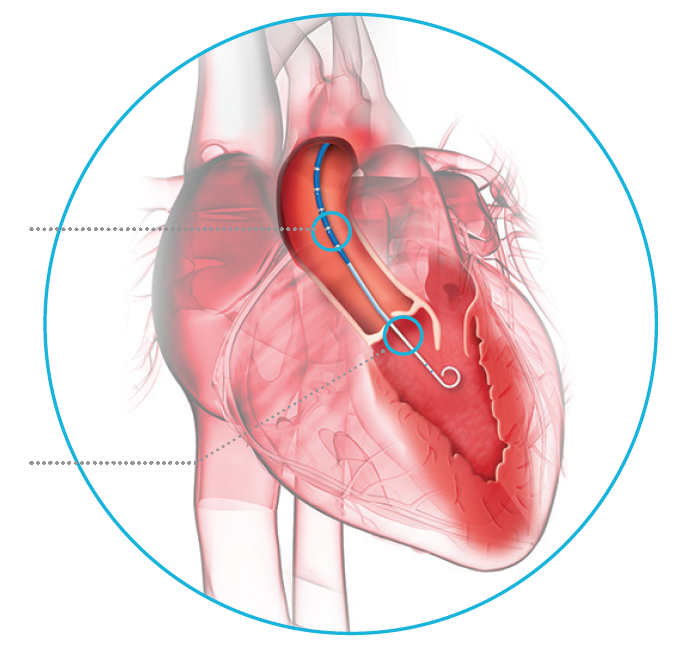
Effigy ane. Placement of Langston Dual Lumen Catheter for simultaneous measurement of differential pressures.
DIAGNOSTIC OPTIONS FOR AORTIC STENOSIS
Noninvasive Tests
Abnormal patterns on an electrocardiogram can reflect a thickened heart muscle and suggest the diagnosis of aortic stenosis. A transesophageal echocardiogram, due to the relative proximity to the center, is more accurate than a standard external echocardiogram, but it requires esophageal coldhearted, conscious sedation, and a brief outpatient stay.
A breast x-ray can show whether the middle shadow is normal or enlarged. Careful inspection of a chest 10-ray sometimes reveals calcification of the aortic valve, but not the extent of the stenosis. An echocardiogram (ultrasound) can show a thickened, calcified aortic valve that opens poorly. Doppler flow tin can exist used to determine the pressure difference on either side of the aortic valve and to estimate the EOA, but it is not always authentic, depending on the skill of the operator and the beefcake of the patient.
Cardiac Catheterization
Cardiac catheterization assists in determining the severity of a valvular stenosis past directly measuring the force per unit area gradient and menses across the valve. In patients with aortic stenosis, a true transvalvular pressure gradient is strongly recommended before valve replacement.
Any catheter designed for ventricular entry tin can obtain a left ventriculogram and measure the pressure inside the left ventricle (LV). However, the Langston Dual Lumen Catheter tin can simultaneously mensurate the pressure in the aorta and the LV.
At that place are several ways that a pressure gradient may exist measured across the aortic valve in a catheterization procedure:
Pullback method. A single-lumen pigtail catheter first measures the LV pressure before a "pullback" of the catheter into the aorta to measure the pressure in the aorta. Measurement is not simultaneous because each is taken during different cardiac beats, which can change the pressures.
Double stick method. Puncturing both groins or radial arteries and placing two pigtail catheters—one in the LV and one in the aorta. This technique produces accurate simultaneous aorta and LV pressures, merely requires bilateral femoral or radial artery punctures, plus the additional introducer sheath, guidewire, and pigtail catheter.
Sidearm of a short sheath. Using a unmarried-lumen pigtail catheter to measure the LV pressure while using the sidearm of the introducer sheath to measure the aortic pressure. This method may be subject to mistaken readings if there is whatsoever iliac or aortic stenosis, which would touch the sidearm pressure reading. Although measuring the slope between the LV and the femoral artery is convenient, downstream augmentation of the pressure point and delay in pressure transmission between the proximal aorta and femoral artery may change the force per unit area waveform and introduce errors.
Sidearm of a long sheath. Using a single lumen pigtail to measure the LV pressure while using the sidearm of a long introducer sheath to measure the aortic pressure. While this technique can yield positive results it can exist difficult and unsafe to run a long sheath through the aorta.
Transseptal Approach. This technique involves a venous approach via a puncture of the ventricular septum with a needle followed by advancement of a catheter into the LV. An additional catheter is placed in the aorta and measures simultaneous pressures at the aortic root. This invasive technique is better suited for patients with mechanical aortic valves due to the want to avoid placing anything across the mechanical valve.
WHY IS ACCURACY SO IMPORTANT?
Because the aortic valve gradient is i of the key measurements used to determine the EOA, which then determines whether valve replacement is performed, it is very important to accurately measure pressures. Physicians demand to exist precise in their diagnostic measurements. The Langston Dual Lumen Catheter, which is designed to simultaneously and accurately measure the pressure gradient across the aortic valve (AV), can help decide the degree of aortic stenosis.
CASE Study: LANGSTON DUAL LUMEN CATHETER
IN Utilize
A 91-yr-sometime woman was referred to the Rechts der Isar Hospital with progressive shortness of jiff and angina at rest for several days. Midsystolic murmur was detected during clinical exam.
Form of treatment
Noninvasive testing with electrocardiogram and echocardiogram showed left ventricular thickening and astringent aortic valve stenosis. The patient was then referred to the cardiac catheterization lab to precisely stage the severity of the underlying aortic valve stenosis. A sheath was introduced into the right radial artery and an AL1 catheter was placed above the aortic valve. A straight wire was used to pass the stenotic aortic valve, and the AL1 catheter was avant-garde into the LV. A J-shaped 0.035-inch wire was so introduced into the LV and the AL1 catheter was removed. The Langston Dual Lumen Catheter was placed into the LV, and simultaneous aortic and ventricular pressure level measurements were obtained.
Results
Due to the simultaneous pressure measurement, a directly and accurate evaluation of the acme-to-peak gradient (62 mm Hg) and mean slope (60 mm Hg) over the aortic valve was found, indicating a high-grade aortic stenosis (Figure 2). Finally, angiography with the Langston Dual Lumen Catheter in the LV showed skilful LV office.

Figure 2. Simultaneous measurement of force per unit area gradients showed a tiptop-to-meridian gradient of 62 mm Hg, and a mean gradient of 60 mm Hg.
Discussion
Accurate and reliable diagnosis and staging of a high-grade symptomatic aortic stenosis was enabled in this case using the Langston Dual Lumen Catheter. Our patient was consequently referred to undergo a successful transcatheter aortic valve replacement.
TIPS FOR Utilise: LANGSTON DUAL LUMEN CATHETER
• Flush both lumens with a heparinized saline solution, and plow the stopcock to a closed position before inserting the catheter into the introducer sheath. If claret is drawn into either lumen, flush lumen immediately to avert jell formation.
• Flush thoroughly and often to remove any air bubbling that may be trapped in the device. Affluent the Langston Dual Lumen Catheter before deployment equally well every bit in one case it is in the eye and to pull the wire (air can be sucked into the system if the wire is removed too quickly).
• When placed appropriately, the sidearm measures the pressure proximal to the valve. The pigtail and multipurpose catheters have a marked "AO" tag on the sidearm to remind the user that it is the aortic force per unit area.
• Transducers should be placed at the same height and the same distance from the center.
• The Langston Dual Lumen Catheter should be normalized/zeroed out prior to crossing the valve to ensure that both lumens are measuring at the same level earlier offset to accept pressures beyond the valve.
• Contrast can bear upon the measured pressure. If an LV angiogram is taken before pulling dorsum, pressure readings may be affected. Flush afterward all contrast injections.
• The sidearm is not designed for power injections and they should not be performed. The tag on the sidearm provides a reminder.
THE LANGSTON DUAL LUMEN CATHETER
Langston Dual Lumen Catheters are angiographic catheters with a two-lumen coaxial-pattern (Figure 3). The inner lumen extends the unabridged length of the catheter and can be used for pressure measurements and power injections. The inner lumen is a standard braided catheter and has an injection pressure rating suitable for Medrad or ACIST injections. The outer lumen terminates three to 15 cm (depending on the version) proximal to the distal finish of the catheter and has a series of sideholes for pressure measurement. The outer lumen has a clear sidearm and three-way stopcock on the proximal end. This lumen is for pressure level measurement only and cannot withstand high pressure level injections. A tag on the sidearm states this alarm.
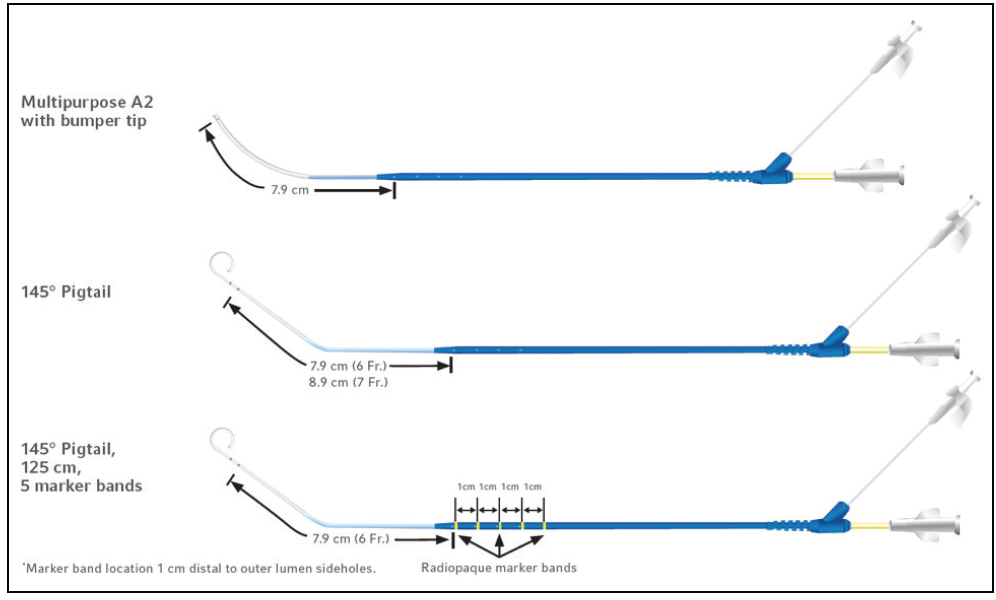
Figure 3. Available Langston configurations.
Deployment
The Langston Dual Lumen Catheter records the force per unit area gradient simultaneously using its coaxial pattern (a lumen within a lumen). The inner braided lumen extends the entire length of the catheter and is positioned in the LV. The catheter tip and multiple sideholes of the inner lumen let for rubber delivery of contrast medium and the transmission of pressures. The outer lumen ends proximal to the distal end of the catheter and is positioned on the proximal side of the aortic valve in the aorta. Although not designed for high pressure injections, the multiple side holes on the outer lumen allow for accurate pressure level manual. The coaxial design allows the pressures from both sites to exist simultaneously measured via external transducers.
ane. Manning WJ. Asymptomatic aortic stenosis in the elderly: a clinical review. JAMA. 2013;310:1490-1497.
two. Otto CM, Prendergast B. Aortic-valve stenosis—from patients at risk to severe valve obstacle. E Engl J Med. 2014;371:744-756.
Indications for Use
Each Langston Dual Lumen Catheter is indicated for commitment of contrast medium in angiographic studies and for simultaneous pressure measurement from two sites. This type of pressure measurement is useful in determining transvalvular, intravascular and intraventricular force per unit area gradients.
Contraindications
The Langston Dual Lumen Catheter is contraindicated for use in:
• synthetic vascular grafts
• bogus heart grafts
Photos from Teleflex Langston Dual Lumen Catheter Brochure # 94 0874 – 00 00 01
Teleflex, the Teleflex logo and Langston are trademarks or registered trademarks of Teleflex Incorporated or its affiliates in the U.Southward. and/or other countries.
Refer to the Instructions for Employ for a complete listing of the indications, contraindications, warnings and precautions.
Langston Dual Lumen Catheters are not available in all regions. Please contact client service to confirm availability in your region.
Source: https://citoday.com/articles/2019-mar-apr/simultaneous-measurement-of-differential-pressures-with-a-dual-lumen-catheter

0 Response to "what is the name of the measuring device used to assess intraventricular pressure?"
Post a Comment